A Spotlight on Lymphoma Awareness Day and the Role of Oncology CROs
September 15, 2024 marks the 20th anniversary of World Lymphoma Awareness Day, a globally recognized event that has raised significant awareness of lymphoma, a type of cancer that affects our lymphatic system. In addition to raising funds for supporting lymphoma clinical research, the 2024 campaign will shed light on the emotional effects of living with lymphoma for both patients and their caregivers, including experiencing anxiety, depression and fear of cancer recurrence or progression.
Every year, joining the efforts of Lymphoma Coalition, the Leukemia & Lymphoma Society, and several other cancer research organizations are the oncology CROs (contract research organizations) who play a crucial role in driving innovative lymphoma clinical research. This is illustrated in the fact that the global in-vivo oncology CRO market size is expected to reach US$2.3 billion by 2030. In their partnerships with oncology sponsors and research institutions, these specialized CROs have been a key component of driving the recent advancements and increased drug approval rates seen in lymphoma clinical trials the last few decades. Recognizing their contributions, this article will highlight the importance of World Lymphoma Awareness Day and discuss the impact of oncology CROs on bridging the gap between lymphoma clinical research and practical, life-saving treatments in clinical settings.
Understanding Lymphoma
How Does Lymphoma Develop?
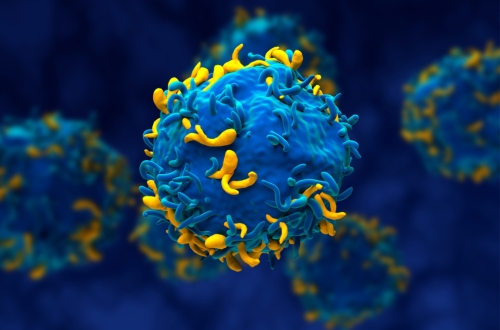
Lymphoma is a type of blood cancer that occurs when tumor cells develop in the lymphatic system, which is a crucial component of the body’s immune system. Normally, this system, made up of lymph nodes, the spleen, thymus gland, and bone marrow, is responsible for fighting infections and diseases. Lymphoma develops when white blood cells (also known as lymphocytes) start to grow abnormally and uncontrollably within these organs and lead to tumors that spread throughout the body.
Types of Lymphoma
There are two main types of lymphoma: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL), each with distinct characteristics and treatment approaches. Differentiating between HL and NHL, as well as determining the specific subtype is critical for determining a patient’s prognosis and treatment strategies. The HL subtype is characterized by the presence of Reed-Sternberg cells, an abnormal type of B-lymphocytes, whereas NHL is an umbrella term of various blood cancers.
Classifying subtypes of NHL is based on the World Health Organization (WHO) system, which groups these diseases based on several criteria:
- The type of lymphocyte (B-cell, T-cell, or other) the lymphoma starts in
- How the lymphoma looks under a microscope
- The chromosome features of the lymphoma cells
- The presence of certain proteins on the surface of the cancer cells
Lymphoma: Prevalence and Global Impact
Lymphoma has a substantial prevalence worldwide, with NHL accounting for 90% of all malignant lymphomas and about 4% of all cancers. Including adults and children, over 8,500 cases of HL and nearly 90,000 cases of NHL are estimated to be diagnosed in the United States throughout 2024. In terms of mortality, the American Cancer Society expects over 900 deaths from HL and more than 20,000 deaths from NHL in 2024 among Americans with lymphoma.
Symptoms and Early Detection
Recognizing the symptoms of lymphoma is important for early diagnosis in patients, which significantly increases the chances of successful treatment and long-term survival. In both HL and NHL, swollen lymph nodes are the most common symptom, often in the neck, armpits, or groin. Others labeled “B symptoms” include fever without an infection, drenching night sweats, and unintentional weight loss.
Patients can experience fatigue, loss of appetite, chest pains, and shortness of breath, but these are non-specific symptoms that can also be associated with other diseases. For this reason, lymphoma can potentially be misdiagnosed, emphasizing the importance of raising awareness and getting regular medical check-ups. When lymphoma is caught early, patients can still have the option to undergo less aggressive treatment options, leading to greater health-related quality of life (HRQoL) and a better prognosis.
Current Treatment Options for Lymphoma
The treatment landscape for lymphoma, in both the HL and NHL subtypes, has improved significantly in recent decades, now offering patients a range of options tailored to their specific type and stage of lymphoma. Many of these treatments can also be combined for maximal efficacy, especially in difficult-to-treat lymphomas.
Traditional Therapies for Lymphoma
There are three main treatment approaches for both the HL and NHL types of lymphoma:
- Chemotherapy: Involves injections of different combinations of powerful anti-cancer drugs that kill tumor cells, but chemotherapy also harms healthy cells.
- Radiation Therapy: Uses high-energy rays (or particles) to target cancer cells with specificity and often follows chemotherapy. Radiation therapy is usually preferred for treating lymphoma that’s completely confined to one area.
- High-dose Chemotherapy and Stem Cell Transplant: Chemotherapy can’t be applied in high doses regularly because of its side effects and severe damage caused to the bone marrow. Stem cell transplants make high-dose chemotherapy possible by replacing the patient’s damaged bone marrow with new blood-forming stem cells.
Targeted Therapies and Recent Advances in Lymphoma Clinical Research
In recent years, there have been remarkable advancements in lymphoma treatment, particularly in the realm of targeted therapies and immunotherapies. These newer approaches aim to attack cancer cells more precisely while sparing healthy tissues, often resulting in fewer side effects compared to traditional chemotherapy.
Immunotherapy helps a patient’s immune system better recognize and destroy cancerous lymphocytes, while sparing healthy tissue. Below are some subtypes of immunotherapy, including individual compounds that are currently approved for use by the US Food and Drug Administration (FDA).
- Monoclonal antibodies: These are manufactured antibodies, which are proteins that help fight infections, designed to attack specific targets only on cancer cells. E.g., brentuximab vedotin, rituxumab.
- Chimeric antigen receptor (CAR) T-cell therapy: T cells are taken from the patient’s blood and are changed in the lab by adding a gene for a receptor (called a chimeric antigen receptor or CAR), which helps the T cells attach to a specific cancer cell antigen. The CAR T cells are then given back to the patient. E.g., tisagenlecleucel, axicabtagene ciloleucel, brexucabtagene autoleucel, lisocabtagene maraleucel.
- Immune checkpoint inhibitors: The immune system regulates itself by maintaining “checkpoints” in the cell cycle to control the immune response. Lymphoma tumor cells can use abnormal checkpoints to avoid being targeted. Checkpoint inhibitors attack PD-1, a protein on T cells that halts their activity, to boost the immune response against cancer cells. E.g., nivolumab, pembrolizumab.
Targeted drug therapy encompasses a large class of drugs with various targeted mechanisms of action that also spare healthy cells, typically used when patients fail traditional therapies. Below are some common classes of targeted therapies, including individual compounds that are currently approved for use by the US FDA
- Proteasome inhibitors: These stop enzyme complexes (proteasomes) in cells from breaking down proteins that are important for keeping cell division under control. E.g., bortezomib.
- Histone deacetylase (HDAC) inhibitors: These target proteins called histones, which interact with DNA chromosomes, to interfere with active genes in cancer cells. E.g., belinostat.
- Bruton tyrosine kinase (BTK) inhibitors: These target the BTK protein, which normally helps some lymphoma cells (B cells) grow and survive. E.g., ibrutinib, acalabrutinib, zanubrutinib, pirtobrutinib.
Personalized Medicine for Lymphoma in Clinical Settings
Advances from lymphoma clinical trials have enabled the emergence of personalized or precision medicine, which allows for therapies to be tailored to the genetic profile of a patient’s cancer. This method is often guided by molecular testing and helps select the most effective treatment unique to each case of lymphoma. With the help of funds raised by World Lymphoma Awareness Day and the efforts of oncology CROs and sponsors within lymphoma clinical research, new therapies and clinical trials are continuously being developed for patients with HL and NHL.
The Role of Oncology CROs in Lymphoma Research
An oncology CRO is an organization that performs a wide variety of clinical research-related duties and functions, including lymphoma clinical trials, for biotech, pharma, and medical device companies. In the context of lymphoma clinical research, these specialized CROs have played a crucial role in driving innovations in cancer drug development, especially because oncology trials are traditionally more complex and challenging than other therapeutic areas. Therefore, successful oncology CROs like TFS HealthScience CRO must possess extensive therapeutic experience in oncology and hematology, as well as navigating the challenges of cancer trials. Lymphoma clinical research sponsors rely on these organizations to help manage and coordinate the operational aspects of the study.
In lymphoma clinical trials, sponsors can outsource one or several of the following study-related tasks, among others, to an oncology CRO.
- Patient recruitment and retention: An experienced CRO will often have an established network of quality investigative sites that can access the patient population of interest, with several approaches in mind to anticipate and overcome enrollment challenges.
- Data management: The CRO is responsible for ensuring data accuracy and integrity and for resolving data queries throughout the clinical trial.
- Centralized monitoring: The CRO conducts regular monitoring visits to clinical research sites, reviewing study documents, performing source data verification (SDV), and ensuring protocol compliance.
- Pharmacovigilance: The CRO is responsible for identifying, evaluating, and reporting any adverse events or side effects that occur during the trial.
- Quality Assurance (QA): The CRO carries out audits and conducts documentation reviews regularly to ensure that the trial is compliant with Good Clinical Practice (GCP) guidelines and ethical regulations.
Case Study: Global CRO Pharm-Olam (Now Allucent) Leads Several Successful Lymphoma Clinical Trials
Many successful lymphoma trials have been led by leading oncology CROs, resulting in breakthrough treatments that have significantly improved patient outcomes. For example, Pharm-Olam, now known as Allucent CRO, has successfully led several lymphoma trials for Infinity Pharmaceuticals over the years. Their collaboration began with the DYNAMO study, focusing on refractory indolent non-Hodgkin’s lymphoma, and has continued with the FRESCO study for relapsed/refractory follicular lymphoma. The expertise of this oncology CRO, as well as their flexibility and dedicated project teams were essential for meeting enrollment goals and advancing investigational medicines developed by Infinity. Read the full article here!
For more case studies, visit our Intellect Hub to discover how TFS Oncology & Hematology CRO delivered success in clinical trials for advanced solid tumors and adoptive cell therapy.
Lymphoma Clinical Trials: The Current Landscape
The current landscape of lymphoma clinical trials demonstrated significant promise at the American Society of Clinical Oncology (ASCO) Annual Meeting 2024, with researchers presenting several exciting findings from ongoing studies. This year’s meeting highlighted the dynamic state of the field of lymphoma clinical research, with the following key lymphoma clinical trials showcasing advances in HL, diffuse large B-cell lymphoma (DLBCL), mantle cell lymphoma (MCL), and natural kill (NK)/T-cell lymphoma (NKTCL).
Pivotal Findings from Recent Lymphoma Clinical Trials
In the clinical treatment landscape of HL, the Phase III GHSG HD21 trial demonstrated that BrECADD (brentuximab vedotin plus etoposide, cyclophosphamide, doxorubicin, dacarbazine, and dexamethasone), a combination therapy, could be a new potential standard of care.
Another ongoing Phase III trial, ECHELON-3, found combination therapy with brentixumab, lenalidomide, and rituximab improves survival outcomes in patients with relapsed or refractory DLBCL.
The Phase I TRANSCEND NHL 001 has been studying the approved CAR T therapy, lisocabtagene maraleucel (liso-cel), for treating patients with MCL. Liso-cel was significantly effective in targeting cancer cells regardless of prior exposure or failure with BTK inhibitor therapies. Although, the benefits of this CAR T-cell agent were greatest in patients who were not resistant to BTK inhibitors and had received under 5 lines of prior therapy.
Lastly, the Phase II CLAMP lymphoma clinical trial found combination therapy consisting of camrelizumab, pegaspargase, etoposide, and high-dose methotrexate may be a promising well-tolerated treatment for patients with NKTCL.
Participating in a Clinical Trial: What to Expect
The process of participating in a clinical trial involves several steps and begins with determining eligibility by reviewing whether a patient meets specific criteria, such as their type and stage of lymphoma, treatment history, and overall health status. Eligible participants then undergo a thorough informed consent process that provides detailed information about the trial’s purpose, procedures, potential risks, and benefits before giving their consent to participate. Despite the uncertainties and potential risks, joining a clinical trial presents a unique opportunity to provide patients with advanced medical therapies and easier access to close monitoring by oncologists. This can be especially valuable for individuals with cancers that are not suited for traditional therapies or do not have many approved treatment options.
Overall, lymphoma clinical trials have been essential for advancing the therapeutic landscape of lymphoma, underscoring the importance of ensuring data from these studies are valid and reliable. Oncology CROs have now become integral for sponsors wanting to optimize data quality, trial efficiency, and market success. From implementing rigorous protocols and monitoring patient safety to collecting and analyzing patient data, CROs specializing in lymphoma clinical research play an important role in delivering new, effective treatments to patients with lymphoma.
The Future of Lymphoma Clinical Research
Oncology CROs and sponsors are leading the road to rapid advancements in lymphoma clinical research, driving several emerging trends for future work. One of the most promising areas is personalized medicine; in recent years, this tailored approach to treating subtypes of lymphoma has been made possible because of advances in genomic sequencing technology and in our understanding of gene changes driving tumor activity in different lymphoma types. The integration of artificial intelligence (AI) and machine learning (ML) are also enabling large-scale data analysis to identify potential new drugs more quickly or for predicting patient responses to lymphoma treatment.
Other areas of focus include developing novel individual CAR T-cell therapies and immunotherapies, like immune checkpoint inhibitors, as well as exploring different combinations of these medications with or without chemotherapy. For example, in July 2024, promising results from a phase 1 Stanford Medicine clinical trial for large B-cell lymphoma led to a breakthrough therapy designation from the FDA for a CD22-directed CAR T-cell agent (read the full article here). For more details on the recent advances in lymphoma clinical research for targeted therapies and immunotherapy in HL and NHL, visit the National Cancer Institute (NCI) here.
Therapeutic resistance is all too common in cancer patients, especially for lymphoma, highlighting the need for investigating multiple promising treatment approaches. Developing new targets, therapies, and approaches benefits patients with HL and NHL and their families by providing additional opportunities for treatment and improved survival outcomes. The oncology CRO and sponsor partnership is crucial for making this happen because they help researchers pool resources, share knowledge, and accelerate innovations in lymphoma drug discovery.
Conclusion
As we approach World Lymphoma Awareness Day on September 15, TFS is joining the ongoing fight against lymphoma to support efforts in raising public awareness about this devastating disease. Promoting patient and caregiver education makes early detection and greater survival possible and several organizations are helping continue lymphoma clinical research deliver new treatments for patients. At the forefront of this mission are oncology CROs like TFS, which have been instrumental in designing and implementing clinical protocols, managing complex data, and navigating regulatory landscapes for lymphoma trials worldwide. From technological advances in genomic sequencing and AI/ML to cutting-edge immunotherapies and targeted treatments, advances in lymphoma clinical research continue to develop, thanks in large part to the rigorous cancer studies managed by these specialized CROs. This World Lymphoma Awareness Day, we encourage readers to engage with awareness initiatives, by supporting ongoing research efforts and considering participating in lymphoma clinical trials when appropriate.
TFS: Your Oncology CRO Partner
TFS HealthScience Oncology and Hematology is dedicated to providing comprehensive services to support your lymphoma clinical trials. With a proven track record of over 300 cancer-related clinical trials across all phases, we’re committed to delivering solutions that match your needs. Our global operations teams are fully experienced with navigating the complex landscape of cancer clinical research, offering rigorous operational oversight and adherence to global standards under the strong leadership of Kris O’Brien, VP, Head of Oncology & Rare Diseases at TFS. Visit our oncology CRO website to learn more or connect with a TFS representative here!
Interested in learning how you can navigate the current landscape of immunotherapy and immune checkpoint inhibitors? Download our white papers and access even more Oncology & Hematology content on the TFS Intellect Hub!
Connect with Us
Contact us today to discover how TFS can be your strategic CRO partner in clinical development.