World Diabetes Day 2024: Spotlight on Promising Clinical Trials
The latest data from the United States (U.S.) Centers for Disease Control and Prevention (CDC) found that nearly 16% of American adults (i.e., 1 in 6 adults) now have diabetes, as of November 2024. Comparatively, the diabetes rates between 1999 and 2000 in the U.S. were significantly lower, at 9.7%. Diabetes is a chronic disease treated in internal medicine that occurs either when the pancreas does not produce enough insulin, termed type 1 diabetes, or when the body cannot effectively use the insulin it produces, known as type 2 diabetes mellitus. Insulin is a hormone that regulates blood glucose, and in uncontrolled diabetes, chronically high blood sugar levels gradually cause serious damage throughout the body, especially the nerves and blood vessels. The damage from diabetes significantly increases the risk of blindness, kidney failure, heart attacks, stroke and lower limb amputation.
Every year on November 14, World Diabetes Day provides an opportunity to raise awareness about diabetes as a critical global public health issue and emphasize the need for greater awareness of prevention and management strategies. As World Diabetes Day 2024 draws near, this blog will highlight the 10 most promising clinical trials pushing the boundaries of diabetes treatment and prevention, from innovative therapies and novel drug delivery methods to breakthroughs in personalized medicine. Continue reading to explore the latest therapeutic advancements aimed at improving the lives of those affected by diabetes and discover how ongoing clinical research is shaping a hopeful future in diabetes care.
1. Phase I, First-In-Human Study Evaluates Stem Cell Therapy in Type 1 Diabetes
ClinicalTrials.gov ID: NCT05210530
Sponsor: ViaCyte, and CRISPR Therapeutics
Location(s): Canada
Description: ViaCyte and CRISPR Therapeutics have collaborated to conduct a clinical study to evaluate the efficacy of a stem cell therapy, named VCTX210, in producing insulin for type 1 diabetes patients. VCTX210 combines pancreatic endoderm cells (PEC210A) which have been genetically modified using CRISPR/Cas9 technology with a perforated device that delivers these PEC210A cells. Other than assessing the safety of this therapy, the trial will determine whether these implanted pancreatic cells can evade immune detection, multiply and differentiate appropriately, and correctly produce insulin to regulate glucose in adults with type 1 diabetes.
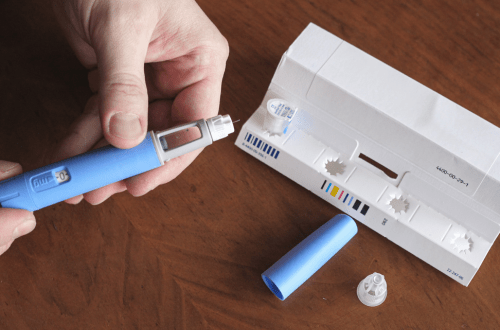
2. Phase IV INHALE-3 Study Investigates the Use of Inhaled Insulin for Type 1 Diabetes
ClinicalTrials.gov ID: NCT05904743
Sponsor: MannKind Corporation
Location(s): U.S.
Description: In June 2024, positive 17-week data from the INHALE-3 clinical trial were shared at the American Diabetes Association’s (ADA) 84th Scientific Sessions in Orlando. Adults with type 1 diabetes participating in this study were randomized to receive one of the following insulin regimens:
- Insulin degludec plus inhaled insulin (Afrezza) combined with continuous glucose monitoring (CGM).
- Usual diabetes care, defined as multiple daily injections (MDI), an automated insulin delivery system, (AID) or a pump without automation.
More participants who received inhaled insulin achieved the trial’s glycemic targets, compared to the usual diabetes care group (30% vs. 17%, respectively). Among those with an A1c (i.e., average blood sugar level over the previous 2-3 months) greater than 7% at baseline, 21% of the inhaled insulin group and 0% of the usual care group were able to lower their A1c percentage to under 7% after 17 weeks. Read the full details of these results in this press release.
3. Early-Phase SECURE-T2D Pivotal Trial Evaluates Automated Insulin Delivery System for Type 2 Diabetes
ClinicalTrials.gov ID: NCT05815342
Sponsor: Insulet Corporation
Location(s): U.S.
Description: The latest data from the SECURE-T2D Phase I/Phase II trial demonstrated the promise of diabetes management technologies in improving glycemic control and quality of life for people with type 2 diabetes. The Omnipod® 5 AID System is a novel insulin pump that automatically adjusts insulin delivery based on CGM data by responding to glucose levels in real-time, reducing such burden from patients themselves. The device was administered for a duration of 13 weeks, after which it resulted in hemoglobin A1c (HbA1c) levels significantly decreasing from a baseline average of 8.2% to 7.4% at the end of the study. Read the full press release here.
Notably, in August 2024, this automated insulin delivery (AID) technology received approval from the U.S. Food and Drug Administration (FDA) for use in adults with type 2 diabetes. This is the first AID system approved for both type 1 and type 2 diabetes management. Read more about this approval here.
4. Phase 1/2 FORWARD Study Reveals Promising Stem-Cell Derived Islet Cell Therapy for Type 1 Diabetes
ClinicalTrials.gov ID: NCT04786262
Sponsor: Vertex Pharmaceuticals
Location(s): U.S., France, Germany, Italy, Netherlands, Norway, Switzerland, the United Kingdom (U.K.)
Description: In June 2024, positive new data from the Phase 1/2 FORWARD clinical trial of VX-880, an infused stem cell-derived islet cell therapy, in people with type 1 diabetes (T1D) with impaired hypoglycemic awareness and severe hypoglycemic events (SHEs). The islet cells can be found in the pancreas and are normally responsible for producing insulin in the body. Notably, this trial’s population consisted of patients who experienced recurrent hypoglycemia episodes, despite receiving appropriate diabetes care. Of the 12 participants for whom new data was available at this time, 11 individuals experienced a reduction in excess insulin at the last study visit (Day 90). During the evaluation period (after Day 90), the occurrence of SHEs was eliminated in all 12 patients. Overall, this clinical trial suggests that stem cell-derived islets regulate blood glucose control as well as natural human islets, making VX-880 a potentially curative therapy for type 1 diabetes. Visit this press release from the ADA to learn more.
5. Artificial Intelligence-Powered Study Enables Personalized Medicine in Type 2 Diabetes Care
ClinicalTrials.gov ID: NCT05181449
Sponsor: The Cleveland Clinic
Location(s): U.S.
Description: In 2022, findings from a clinical study driven by artificial intelligence (AI) in type 2 diabetes were presented at the 82nd Scientific Sessions of the ADA, demonstrating how Whole Body Digital Twin™ technology enables personalized medicine in diabetes care. The Whole Body Digital Twin™ is a platform that uses AI to build a dynamic model that represents each individual’s unique metabolism. The tool is trained by data collected on a daily basis from the patient’s wearable sensors, clinical lab results, and self-reported outcomes. Learn more about this AI-powered technology in this press release.
In its randomized clinical trial, participants with type 2 diabetes were cared for using the Twin Precision Treatment technology (TPT) versus standard of care. The TPT intervention used the Whole Body Digital Twin™ app to provide personalized coaching on nutrition, sleep, activity, and breathing to reduce A1c levels and promote disease remission. At interim analysis after 180 days, 94.9% (189/199) of TPT patients achieved an A1C less than 6.5% on no medications or metformin only, while 83.9% (167/199) achieved clinical diabetes remission. Read the full study results here. More recently, in December 2023, the creators of the Whole Body Digital Twin™ service, Twin Health, secured US$50 million in funding to expand this technology for the prevention of chronic metabolic diseases.
6. Phase I PROVENT Trial Highlights the Potential of a Vaccine for Type 1 Diabetes
ClinicalTrials.gov ID: NCT04690426
Sponsor: Provention Bio
Location(s): Finland
Description: Earlier this year in February, Hyöty et al. (2024) reported results from a phase I study that tested the safety, tolerability, and immunogenicity of PRV-101, a multivalent vaccine that targets coxsackie B viruses (CBVs) associated with type 1 diabetes. Healthy adults were randomized into the trial and received either placebo, low-dose PRV-101, or high-dose PRV-101. Among the 32 participants treated, no serious adverse events or adverse events leading to study treatment discontinuation were observed. Treatment with the PRV-101 vaccine demonstrated sufficient immunogenicity; after 24 weeks of post-dose follow-up, protective titers against all five serotypes were seen in more than 90% of participants in the low- and high-dose groups. These results support further evaluation of PRV-101 as a possible vaccine to eliminate one known trigger for type 1 diabetes. Read more about the PROVENT trial and diabetes-associated CBV here.
7. ZOE METHOD Trial Compared Personalized vs. Generalized Nutrition for Prediabetes
ClinicalTrials.gov ID: NCT03222791
Sponsor: Zoe Global Limited
Location(s): U.S.
Description: The results of the ZOE METHOD randomized controlled clinical trial were released in this 2024 publication from Bermingham et al. Nearly 350 adult participants from the U.S. were enrolled and received either a personalized dietary program (PDP) or general advice (control). The effect of both approaches to nutrition on cardiometabolic health, including prediabetes, was then assessed by the study outcomes. After 18 weeks, those within the PDP regimen arm saw significant improvements in their triglyceride levels, relative to baseline measurements, as well as in secondary outcomes such as body weight, waist circumference, HbA1c, diet quality, and microbiome. These results suggest that, rather than opting for a one-size-fits-all approach to nutrition in diabetes care, adopting a personalized approach may be more effective for treating prediabetes and type 2 diabetes indirectly by improving weight and cardiometabolic health.
8. Tirzepatide Significantly Reduces Risk of Type 2 Diabetes in SURMOUNT-1 Trial
ClinicalTrials.gov ID: NCT04184622
Sponsor: Eli Lilly and Company
Location(s): U.S., China, India, Japan, Mexico, Puerto Rico, Russian Federation, Taiwan
Description: In August 2024, Eli Lilly and Company shared positive topline results from their Phase III SURMOUNT-1 clinical trial, which evaluated the efficacy and safety of tirzepatide over 176 weeks in adults with prediabetes and obesity. The trial results showed that weekly tirzepatide injections (at doses of 5 mg, 10 mg, and 15 mg) significantly reduced the risk of progression to type 2 diabetes by 94% among adults with prediabetes and obesity or excessive weight compared to placebo. The treatment also resulted in noticeable weight loss during the study period, with patients who received 15 mg tirzepatide experiencing a 22.9% average decrease in body weight compared to 2.1% in the placebo group. By the 17-week off-treatment follow-up period, patients in the experimental arm overall had an 88% reduction in the risk of progression to type 2 diabetes compared to placebo. These latest results from the SURMOUNT-1 demonstrate the strong potential of tirzepatide to act as an effective intervention for patients with prediabetes.
9. Dexcom CGM Provides Long-Term Glycemic Improvement in Type 2 Diabetes
Publication DOI: https://doi.org/10.1089/dia.2024.0197
Sponsor: Dexcom, CGParkin Communications, International Diabetes Center
Location(s): U.S.
Description: At this year’s ADA Scientific Sessions, DexCom revealed additional clinical data from several studies on their Dexcom CGM, a real-time CGM device for those with type 2 diabetes. Among the data presented, this real-world study demonstrated the benefits of this CGM device in patients with sub-optimally controlled non-insulin-treated type 2 diabetes, reporting improvements in A1C independent of anti-diabetes medication. Dexcom CGM was associated with increased time in range (TIR), a glycemic metric that represents how long a patient is within an appropriate blood sugar range. At 12 months, the proportion of CGM users who met the target TIR of >70% increased from 0% to 43.9% in the <65 years old cohort and from 0% to 37.4% in the ≥65 years old cohort (P = 0.008). Therefore, real-world data (RWD) on Dexcom CGM suggests the device provides long-term glycemic improvements in patients with non-insulin-treated type 2 diabetes.
Another study also reported that Dexcom CGM may be a valuable diabetes prevention tool for individuals with prediabetes by promoting healthy lifestyle changes. It reported that CGM use was associated with improvements in nutrition habits, physical activity, weight, blood pressure, worry, energy levels, and healthcare provider interactions. Read more about the latest clinical findings for Dexcom CGM from ADA 2024 here.
10. Investigator-Initiated Trial Successfully Prevents Islet Transplant Rejection in Adults with Type 1 Diabetes
ClinicalTrials.gov ID: NCT06305286
Sponsor: University of Chicago, Eledon Pharmaceuticals
Location(s): U.S.
Description: In October 2024, researchers from the University of Chicago Medicine Transplant Institute announced potentially the first human cases of insulin independence and glucose control in islet transplant recipients with type 1 diabetes. The three patients were treated with tegoprubart, an anti-CD40L monoclonal antibody. The first two islet transplant recipients achieved insulin independence and normal blood glucose control post-transplant. The third subject had only recently received an islet transplant, but tegoprubart successfully decreased insulin use by more than 60% within three days post-procedure, suggesting they will also eventually reach insulin independence.
Type 1 diabetes is characterized as an autoimmune condition in which patients lose their ability to produce insulin effectively because the pancreatic islet cells have been abnormally targeted by the immune system. Pancreatic islet transplantation involves engraftment with insulin-producing beta cells isolated from the pancreas of another human donor. Following the transplant, patients with type 1 diabetes can theoretically produce insulin on their own without the need for insulin injections, but only if the foreign islet cells are not rejected. This is where immunosuppression treatment with tegoprubart is necessary because it prevents transplant rejection, allowing the patient to achieve insulin freedom. The first islet cell therapy, Lantidra, was approved by the U.S. FDA only recently in 2023, meaning more studies are needed before this rare form of therapy for type 1 diabetes can become more widespread.
Conclusion
In conclusion, the ten innovative clinical trials we have spotlighted here represent cutting edge research taking place in internal medicine and diabetes care in 2024. Although several are still ongoing and the full impact of these novel therapies are not yet seen, they do demonstrate how rapidly new treatment options and even potential curative therapies for diabetes are emerging. As we approach World Diabetes Day 2024 on November 14, join TFS in celebrating the tireless efforts of endocrinology researchers, healthcare professionals, as well as the patients who make these clinical trials possible. Learn more about this year’s campaign from the World Health Organization here.
About TFS CRO: Your Industry Partner in Internal Medicine Clinical Trials
TFS HealthScience is a global CRO (contract research organization) pioneering the future of internal medicine and diabetes care under the leadership of Vice President Anne-Marie Nagy, Ph.D., a specialist in internal medicine indications. Named one of the top 10 influential women in clinical research, Dr. Nagy has guided the Internal Medicine CRO at TFS to amass an impressive track record, including over 350 clinical studies conducted in just the past five years and nearly 500 phase I-IV clinical trials supported in internal medicine and related areas.
Our global expertise and high-quality clinical development services have established us as a trusted partner for clinical trials in any country across several therapeutic areas in internal medicine, including Cardiovascular, Endocrinology/Metabolics, Gastroenterology, and Respiratory/Pulmonology. When you choose TFS as your CRO partner, you choose passion, quality, and a trustful collaboration. Connect with TFS HealthScience CRO on LinkedIn or speak with a TFS representative here today!
Interested in more internal medicine content from us? Visit the TFS Intellect Hub for additional resources, including articles, white papers, case studies, and more!
Connect with Us
Contact us today to discover how TFS can be your strategic CRO partner in clinical development.