Exploring the Link Between Microvascular Capillary Abnormalities and Primary Open-Angle Glaucoma
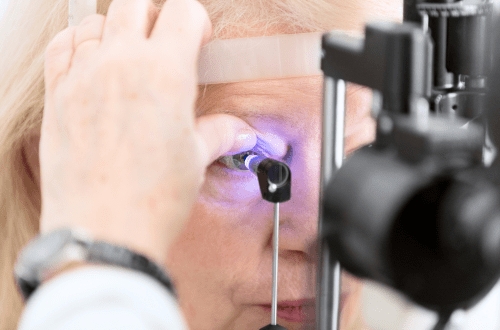
Glaucoma is the leading cause of irreversible vision loss globally, with various etiologies, including vascular abnormalities, implicated in glaucoma pathogenesis. Primary open-angle glaucoma (POAG) or open-angle glaucoma is a multifactorial progressive optic neuropathy, resulting in retinal ganglion cell (RGC) death, distinctive morphological changes to the optic nerve head (ONH), and thinning of the retinal nerve fiber layer (RNFL). Patients develop distinctive visual field defects, which can worsen to irreversible blindness.
Despite years of research, the complex pathogenesis of POAG has yet to be fully elucidated. However, recent studies indicate a complex pathogenesis, with increasing attention on the role of microvascular capillary abnormalities.
This article explores the growing evidence linking these vascular irregularities to POAG, highlighting the importance of understanding this relationship for advancing clinical research and treatment approaches.
Elevated IOP & Ocular and Systemic Vascular Risk Factors
The only modifiable POAG risk factor is elevated intraocular pressure (IOP); however, elevated IOP does not explain why patients with normal IOP get glaucoma. Additionally, some glaucoma patients with adequate IOP control still experience disease progression. Growing evidence suggests that ocular and systemic vascular risk factors play a role in the development of glaucoma and that a reduction in ocular blood flow may cause ischemic damage and lead to RGC death and structural changes in the ONH. Furthermore, decreased ocular perfusion pressure (OPP; calculated from blood pressure and IOP) may lead to poor retinal microvascular perfusion and, ultimately, disease progression.
Risk Factor – Family History
A study by Bayraktar et al. compared the radial peripapillary capillary vessel density (RPCVD) and peripapillary retinal nerve fiber layer (RNFL) thickness values in healthy adult children of patients with primary open-angle glaucoma (POAG) and age-matched healthy controls without a family history of POAG. They found that despite the two groups having similar RNFL thickness values, the eyes of adult children of patients with POAG had significantly lower RPCVD than the controls. The observed decrease in RPCVD indicates potential early microvascular alterations in the eyes of the at-risk individuals. Separately, a study investigated microvascular changes in optic disc, peripapillary, or macular regions in healthy subjects with a family history of glaucoma. Compared to controls, the first-degree relatives of POAG patients had significantly greater inter-eye asymmetry in superonasal peripapillary vessel density (VD) and less VD in the lower nasal peripapillary region, without any detectable clinical, structural, and functional changes.
Risk Factor – Cardiac surgery
Vičaitė et al. investigated the effect of an impaired cardiovascular supply on the structural and vascular parameters of the retina by comparing POAG patients and patients undergoing cardiac surgery with cardiopulmonary bypass. They found that the latter had reduced optic nerve head (ONH) VD, similar to patients with POAG. However, differences in the topographic location of the structural damage and the relationship between structural and hemodynamic parameters in the two groups suggest potentially different impacts from VD reductions. They concluded that significant cardiovascular disease may elevate the risk of POAG, or the VD loss in both groups may be due to distinct pathophysiologic mechanisms, and suggest further investigation. Regardless, they recommend that clinicians keep in mind the importance of non-IOP-related risk factors when managing glaucoma, as they might also influence disease progression.
Is Primary Open-Angle Glaucoma a Vascular Disease?
Using the new technology, Adaptive Optics, a recent study assessed the relationship between retinal arteriolar morphology and glaucoma severity in patients with POAG at different stages. This technology enables the analysis of retinal vasculature at the cellular level in vivo. The study findings suggest that vascular dysfunction is present in POAG, even at a very early stage of glaucoma, and increases with disease severity.
While research on ocular perfusion pressure and other factors affecting blood flow to the eye has grown in recent decades, more attention should be paid to the blood vessels themselves. Landis et al. found only two studies in the past 50 years, both of which reported decreased blood VD in glaucoma. Adding to this finding, the researchers reported reduced blood vessel numbers in the superolateral quadrant of a glaucomatous individual’s ONH. Together, their findings raise the possibility that individuals with a relatively sparse ONH blood supply are more likely to develop glaucoma, recommending further studies with larger sample sizes.
A recent cross-sectional study by Taniguchi et al. investigated peripheral microvascular abnormalities associated with patients with POAG compared with controls. All participants underwent detailed ophthalmic evaluations, including the Humphrey visual field tests. Nailfold capillaroscopy and laser Doppler imaging were also performed. The main outcome measures were the presence of microhemorrhages, tortuous capillaries, dilated capillaries, avascular areas, and capillary density, amongst others. The authors concluded that significant peripheral microvascular abnormalities were found in patients with POAG compared to controls, suggesting that microvascular changes might play a role in glaucoma pathogenesis.
Vascular Abnormalities and Glaucoma – What Comes First?
A recent review aimed to investigate published evidence concerning the relationship between vascular abnormalities and glaucoma and provide an overview of the “chicken or egg” dilemma. Wang et al. identified biomarkers of glaucoma progression from a vascular perspective, including endothelin-1 (ET-1), nitric oxide, and vascular endothelial growth factor (VEGF). They assessed their potential as pharmacological intervention targets. While it is increasingly apparent that vascular abnormalities are closely associated with observed neurodegeneration in glaucoma, the authors caution that it is essential to recognize that glaucoma itself can initiate retinal vascular abnormalities. They concluded that, given the multifactorial nature of the disease, vascular abnormalities represent just one of many contributing factors to the neurodegenerative processes.
Novel Intervention – HIT Training to Improve Microvascular Function
A study protocol describes an exciting approach to glaucoma: high-intensity interval training (HIT training) as an add-on treatment to usual patient care. Highlighting the findings of previous studies, which indicate that approximately one-third of patients experience disease progression despite effective IOP reduction, Van Eijgen et al. are exploring the potential of exercise training to counteract the microvascular endothelial function, chronic inflammation, and oxidative stress that affect retinal neuronal networks, and associated with glaucoma severity and progression. They hypothesize that exercise therapy will improve retinal microvascular function and, thus, ocular blood flow in patients with glaucoma.
The Role of Clinical Research in Understanding Primary Open-Angle Glaucoma
Clinical research in ophthalmology, particularly through specialized Ophthalmology CROs, is essential for exploring the vascular aspects of POAG. Studies focusing on the relationship between vascular health and glaucoma are critical for developing targeted therapies. The integration of advanced imaging techniques and artificial intelligence, as discussed in three ways AI is revolutionizing ophthalmology, is enhancing the precision and effectiveness of glaucoma research.
Advancing Glaucoma Research: OCTA and Computational Methods
Optical Coherence Tomography Angiography (OCTA) in Glaucoma
A recent article highlights the role of optical coherence tomography angiography (OCTA), a non-invasive imaging modality for visualizing ophthalmic microvasculature, in glaucoma. Blood flow is used as a contrast agent to distinguish blood vessels from surrounding tissue. Vessel density is primarily used to quantify ophthalmic microvasculature. Key anatomic regions for OCTA are the ONH area, including the peripapillary and macular regions. OCTA technology can evaluate and monitor glaucoma. Overall, OCTA plays a complementary role in structural optical coherence tomography (OCT) imaging and visual field testing to aid in diagnosing and monitoring glaucoma.
Advanced Computational Methods in Glaucoma Research
Advancements in computational techniques have transformed glaucoma research in recent years. For instance, systems genetics integrates genomic and clinical data, to identify drug targets, understand disease mechanisms, and tailor treatment strategies for glaucoma. Artificial intelligence (AI) technologies can revolutionize glaucoma research by enhancing disease diagnosis, target identification, and drug candidate selection. Computational methods work harmoniously together to discover novel ways to combat glaucoma.
Conclusion and Key Developments in Ophthalmology for 2024
The association between microvascular capillary abnormalities and primary open-angle glaucoma underscores the need for continued research in this area. By focusing on the vascular components of glaucoma pathogenesis, we can advance our understanding and treatment of this complex disease.
As the biotechnology and ophthalmology sectors continue to intersect, new developments are emerging that could significantly impact POAG treatment. Innovations in drug delivery systems and novel therapeutic approaches are paving the way for more effective management of glaucoma. For an in-depth look at these advancements, read our article on key developments for 2024.
TFS: Your Global Ophthalmology CRO Partner
TFS HealthScience (TFS) is a global, mid-size contract research organization (CRO) serving biotech and pharmaceutical companies. Our Ophthalmology CRO Business Unit leads ophthalmic clinical research and provides comprehensive CRO services across the entire spectrum of ophthalmology studies. TFS offers extensive experience and resources for customized ophthalmic clinical research solutions. We integrate internal scientific, medical, regulatory, and operational expertise with innovative technology and a network of trusted resources to expedite your product’s journey to market. Learn more about TFS’s expertise in Ophthalmology and meet our dedicated ophthalmology team.
Our cutting-edge methodologies and global reach establish us as a trusted partner for biotech and pharmaceutical companies. To discover more about our capabilities, view our indication knowledge, and see the global ophthalmology clinical trials we’ve completed, download our one-pager on TFS’s expertise in Ophthalmology.
For further inquiries or to request a proposal, contact a team member. Let’s collaborate to bring innovative solutions to the field of ophthalmology.
Connect with Us
Contact us today to discover how TFS can be your strategic CRO partner in clinical development.