Genetic Factors and Breast Cancer: What You Need to Know
More than 360,000 individuals, both men and women, will be diagnosed with breast cancer in 2024. This type of cancer occurs when cells within breast tissue begin growing uncontrollably, forming tumors. Globally, in 2022, the World Health Organization (WHO) reported that breast cancer was the most common cancer in women in 157 countries and resulted in 670,000 deaths the same year. To recognize the significant burden of this disease, with over 2 million women diagnosed worldwide in 2022, October marks Breast Cancer Awareness Month each year. During this time, patients, families, healthcare organizations, research sponsors, and oncology CROs (contract research organizations) come together to shed light on this devastating disease.
When detected early, the 5-year relative survival rate of breast cancer is 99%, but this is only possible by spreading awareness and promoting action. This year, TFS HealthScience is joining the National Breast Cancer Foundation’s mission of Helping Women NowⓇ by bringing attention to the complexities of breast cancer. In this article, we will take a look at the role of genetic factors in this disease, understanding its role in breast cancer development, diagnosis, and treatment. Read on to learn about the genetics of breast cancer!
Back to Basics: What are Genetic Mutations?
Every cell in the human body is composed of genes; each gene contains a set of instructions, or a genetic code, that dictates everything from cellular processes to how we look. This information also controls how our cells grow, divide, and die, which is why when certain genes become mutated, cell growth can become uncontrolled and result in cancerous tumors. Mutations occur when changes in the genetic code affect the function of the gene, but as a whole, these are relatively rare. The information in genes is inherited and can be passed onto your children; similarly, changes or mutations to genes can be shared among family members. Therefore, some people can have a genetic predisposition to certain diseases because specific genetic mutations have proven to be linked to a higher risk of diagnosis. Although not all types of breast cancer are hereditary, between 5% to 10% of cases in the United States (U.S.) are related to a known inherited gene mutation.
Understanding Genetic Predisposition to Breast Cancer
Family history of breast cancer is known to be one of the strongest risk factors for breast cancer. Several genes have been identified to confer a greater risk of the disease, but the two most important and well-known are the BRCA1 and BRCA2 (BReast CAncer genes 1 and 2). Everyone has these tumor suppressor genes, and when functioning normally, they prevent cells from growing uncontrollably and help repair DNA damage. Mutations in one or both the BRCA1/2 genes can be inherited and increase an individual’s (both in men and women) risk of breast cancer.
Overall, the lifetime risk of developing breast cancer in women in the U.S. who have a BRCA1/2 inherited gene mutation is 60%, in contrast to those without, who have a lifetime risk of 8%. However, 0.2-1.2% of men with an inherited BRCA1 mutation and 1.8-7.1% of those with an inherited BRCA2 mutation will develop breast cancer by age 70. When comparing BRCA1 versus BRCA2, the National Breast Cancer Foundation states 55-65% of women with the BRCA1 mutation will develop breast cancer before age 70, whereas this risk is lower at 45% in women with the BRCA2 mutation. BRCA1/2 mutations are also associated with pancreatic cancer and melanoma (BRCA2 gene mutations only) in men and women, as well as prostate cancer in men.
Besides BRCA1/2, mutations in several genes have been linked with a moderate to high risk of breast cancer: TP53, PTEN, CDH1, ATM, CHEK2, PALB2, RAD51C, RAD51D, NF1, and MSH6. Others are also under study and may play a role in increasing susceptibility to breast cancer, but BRCA1/2 remain the most strongly associated inherited gene mutations.
The Impact of Genetic Factors on Breast Cancer Diagnosis and Prognosis
Genetic factors not only influence the risk of developing hereditary breast cancer types, including early onset breast cancer (EOBC), but also play a crucial role in timely diagnosis and improved prognosis. When a patient is diagnosed, genetic information can provide valuable insights into the tumor’s behavior and guide treatment decisions from the clinician’s perspective. This is because certain genetic mutations are known to be associated with more aggressive forms of breast cancer.
BRCA1-related breast cancers are more likely to be triple-negative, which describes tumors that lack receptors for estrogen, progesterone, and HER2 protein. As a result, triple-negative cancers tend to grow more quickly and have fewer targeted treatment options. In contrast, the majority of patients with BRCA2-related breast cancers will have tumors positive for estrogen receptor expression, which expands the number of available therapies. Although some emerging evidence suggests that women with BRCA2 mutations may have a worse prognosis than those with BRCA1 mutations or with sporadic breast cancer, potentially due to higher recurrence rates. However, survival rates from breast cancer as a whole have improved due to advancements in diagnostic and treatment modalities, with noninvasive forms of the disease showing 90% and 84% survival rates at 5 and 10 years, respectively.
Genetic Testing: A Tool for Risk Assessment and Prevention
A key reason for improvements in early breast cancer detection and diagnosis has been the rise of genetic testing for identifying high-risk individuals. To date, BRCA1/2 are the primary genes of interest and genetic testing ensures harmful changes in these genes are detected accurately. According to the National Cancer Institute (NCI), genetic counseling and testing to determine BRCA1/2 status are recommended for adults with the following risk factors:
- Having a family member with an inherited harmful change in the BRCA1 or BRCA2 gene
- Having Ashkenazi Jewish heritage
- Having a personal or family history of breast cancer at age 50 or younger
- Having a personal or family history of ovarian cancer, male breast cancer, pancreatic cancer, or metastatic or high-risk prostate cancer
How is BRCA1/2 Genetic Testing Done?
Because BRCA1/2 are found in every cell in our bodies, detecting DNA mutations in these genes can be done using either blood or saliva samples from patients. The American Cancer Society (ACS) states that genetic testing can look for one or multiple specific mutations in the BRCA1/2 genes, or more extensive testing can be done to look for many different BRCA mutations. Once tested, the results can come back as either positive or negative for the mutation(s) tested, inconclusive, or positive for a variant of unknown significance (VUS). A VUS is a gene change that has been detected, but it is unknown whether it will affect your risk of developing breast cancer.
It is important to note that a positive result does not mean that the patient is guaranteed to develop cancer, only that they have a higher risk and may require more frequent screenings or preventative measures. Similarly, negative results are reassuring but do not mean there is zero chance of developing cancer in the future. Overall, getting genetic testing done is a patient’s personal choice and any test results should be discussed with a trained healthcare professional in the context of the individual’s overall health and family medical history.
Screening Recommendations from the American Cancer Society
Genetic testing is only one component of screening processes recommended by the ACS for helping detect and diagnose breast cancer. Other methods include mammograms (low-dose x-rays done on breast tissue), as well as regular physical breast exams done by either a health professional (clinical breast exams) or by women themselves (breast self-exams). However, the evidence supporting whether regular physical exams help find breast cancer early is still inconclusive. The ACS also presents different screening guidelines for those who are at average risk of breast cancer versus those at high risk. See this article for more information on recommended screening guidelines from the American Cancer Society.
Gene Therapy: A Promising Frontier in Breast Cancer Treatment
Beyond the role of genetics in understanding breast cancer, as well as detecting and diagnosing it, it can also guide oncology treatment approaches like gene therapy. Gene therapy is a type of cancer treatment that uses the delivery of genetic materials through vectors to target cells in a tumor to correct or modify specific genetic abnormalities. Although this type of treatment is still in its early stages, many strategies have entered human testing in breast cancer clinical trials. Visit Table 2 in this 2023 publication by Wang and Wu for a recent list of clinical trials ongoing for gene therapy in breast cancer.
Genetic information is used to identify patients who might benefit from specific targeted therapies, including in the context of clinical trials for experimental oncology therapies. Tests like Oncotype DX, MammaPrint, and Prosigna can capture a patient’s unique gene expression profile. These are primarily used in the case of EOBC, but they can provide clinicians with information about the likelihood of cancer recurrence and whether chemotherapy is a suitable option for reducing the chances of recurrence.
As another example, this 2020 study by Martínez-Sáez et al. analyzed over 6,300 patients with breast cancer and found that 35.7% of cases had tumors with mutations in the PIK3CA gene. Therefore, these patients could be eligible for treatment with targeted therapies like Itovebi (inavolisib), which is a highly selective inhibitor of the PI3K alpha isoform approved by the U.S. Food and Drug Administration (FDA) in October 2024. Itovebi in combination with palbociclib and fulvestrant is indicated by the FDA for treating adults with endocrine-resistant, PIK3CA-mutated, HR-positive, HER2-negative, advanced breast cancer.
The Future of Breast Cancer Clinical Research in Oncology
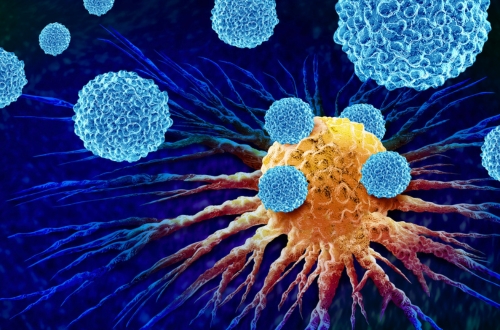
As the field of oncology evolves with new advancements in biotechnology, breast cancer clinical researchers are exploring several new uses for gene therapy in the future. In individuals with mutated BRCA1 or BRCA2 genes, delivering functional copies to replace the abnormal copies in cancer cells may help reverse the effects of inherited harmful gene changes. Additionally, CRISPR-Cas9 technology has recently begun to be investigated as a method for directly repairing mutated genes in breast cancer cells. Finally, gene therapy techniques can complement immunotherapy by improving the immune system’s ability to recognize and attack cancer cells. For example, in CAR T-cell therapy, a patient’s immune T cells can be genetically modified to target specific antigens expressed by a patient’s unique tumors. Overall, gene therapy for breast cancer is still undergoing experimentation in preclinical and clinical testing phases. Nonetheless, it is a promising new opportunity in the field of oncology for treating patients with more personalized therapies, especially for those who are genetically predisposed to hereditary conditions like breast cancer.
Conclusion
This October, join TFS Oncology CRO as we commemorate Breast Cancer Awareness Month and spread awareness about the genetic factors influencing the prevention, early detection, and treatment of breast cancer. Individuals with certain inherited harmful mutations in genes like BRCA1/2 are at a higher risk of developing the disease, but this is by no means a sealed fate. Education around common risk factors can still empower high-risk individuals to be proactive about their health by implementing regular screenings (e.g., mammograms and genetic counseling), lifestyle modifications (e.g., healthy eating and regular exercise), and open communication with healthcare professionals can make a difference in managing breast cancer risk. The field of oncology is seeing an ongoing shift towards personalized medicine, also known as precision medicine, and gene therapy is playing a crucial role in advancing these approaches for patients living with breast cancer.
To learn about how you can support the National Breast Cancer Foundation this Breast Cancer Awareness Month, visit their website and discover various ways of Helping Women Now®.
TFS Oncology CRO: An Industry Leader in Supporting Breast Cancer Research
TFS’ Oncology and Hematology services are dedicated to providing comprehensive support for your breast cancer clinical trials, both local and global. With a proven track record of over 300 cancer-related clinical trials across all phases, our global operations teams are fully experienced with navigating the complex landscape of cancer clinical research. TFS offers rigorous operational oversight and adherence to global standards under the strong leadership of Kris O’Brien, VP, Head of Oncology & Rare Diseases. Visit our oncology CRO website to learn more or connect with a TFS representative here!
Interested in more Oncology and Hematology CRO content from TFS? Visit our Intellect Hub here to access white papers, articles, case studies, and more!
Connect with Us
Contact us today to discover how TFS can be your strategic CRO partner in clinical development.